Living with inflammatory bowel disease (IBD) is a bit of a rollercoaster, there’s uncertainty, lots
of questions, and honestly, no shortage of frustration about what the future holds. Millions of
folks worldwide deal with this chronic illness—whether it’s Crohn’s disease or ulcerative colitis,
and most of us have wondered at some point if true, lasting relief is even possible.
There’s no actual cure for inflammatory bowel disease, but modern treatments can do a pretty
good job of managing symptoms and helping people enjoy long stretches of remission. That
might sound a bit discouraging at first, but honestly, things are a lot more hopeful than they used
to be. With the advances in medicine these days, there are all kinds of ways to control
inflammation, cut down on symptoms, and keep your quality of life up where it belongs.
So, what actually causes IBD? How long does it stick around? Can you live a “normal” life with
it? We’ll get into all that, plus a rundown of current treatment options, strategies to handle daily
life, and some thoughts about diet, stress, and those nagging worries about complications.
Knowing what you’re up against (and what you can do about it) really does help you take charge
of your own health.
What Causes Inflammatory Bowel Disease?
No one really knows for sure what causes inflammatory bowel disease, but it’s likely a mix of your genes and certain environmental factors that push your immune system into overdrive.
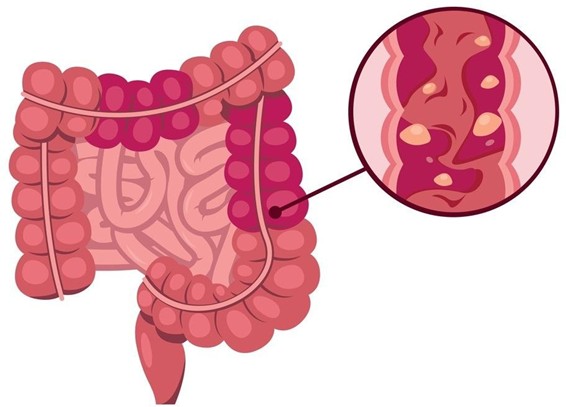
Immune System Dysfunction With IBD, your immune system gets a little too enthusiastic and attacks healthy cells in the gut. The result? Chronic inflammation in the digestive tract. That inflammation messes with normal bowel function and brings on the classic symptoms you see in both ulcerative colitis (UC) and Crohn’s disease (CD).
Key Contributing Factors:
| Factor | Description | Genetic predisposition | Family history increases risk significantly |
| Environmental factors | Diet, stress, infections may trigger onset |
| Immune dysfunction | Overactive immune response targets healthy tissue |
| Gut bacteria | Imbalanced microbiome may contribute to inflammation |
Genetic vs Environmental Influences
There’s no denying that genetics matter a lot. If IBD runs in your family, your odds go up. But it’s not the whole story.
Environmental stuff like what you eat, whether you smoke, stress levels, and certain infections probably act as the match that lights the fire for folks who are already genetically at risk.
Western diets, lots of antibiotics, and even less exposure to certain bacteria as kids might all play a part.
Both ulcerative colitis and Crohn’s disease have a lot in common underneath it all, but they hit different parts of the gut and might react differently to whatever triggers are floating around.
How Long Does Inflammatory Bowel Disease Last?
IBD is a chronic, lifelong thing. It’s not something that just goes away, and managing it is usually a long-term commitment.
Disease Pattern
IBD usually follows a pattern of ups and downs, with periods of active symptoms known as flares, followed by stretches of relief when the condition goes into remission. During flares, you might deal with nasty abdominal pain, diarrhoea, and all sorts of other annoyances.
Some people find their IBD eases up a bit after age 60, but for plenty of others, symptoms stick around. That “burned out” phase you might’ve heard about? It’s pretty rare, honestly.
Symptom Duration
IBD symptoms can be all over the map,sometimes they’re mild and short-lived, other times they drag on for weeks or months. Remission can last years for some, but not for everyone.
The unpredictability is frustrating. Abdominal pain and other IBD symptoms can pop up out of nowhere when you least expect it.
Long-term Management
Most people need ongoing medication to keep things under control and hopefully cut down on the number of flares. There’s no cure, but with the right treatment, you can manage it pretty well.
Regular check-ins with your doctor are a must. Treatment plans often change as your symptoms do, so flexibility is key.
Can You Live A Normal Life With Inflammatory Bowel Disease?
With the right treatment living with IBD can feel much like any other life. IBD definitely impacts quality of life, but there are solid ways to keep it from taking over.
Physical symptoms ebb and flow. Sometimes they’re barely noticeable, especially during remission, so you can get on with work, hobbies, social stuff—pretty much whatever you’d do otherwise.
Some things that help keep life on track:
- Sticking to your treatment plan (even when you feel fine)
- Checking in with IBD specialists regularly
- Managing symptoms before they get out of hand
- Keeping an eye on flares and acting fast
Everyone’s IBD journey is different. Some folks barely have symptoms for years, others deal with more frequent ups and downs.
Mental health is a big one. Depression and anxiety are pretty common among IBD patients, and they can make everything feel tougher.
Sure, flares can throw a wrench in your plans and disrupt daily life. But between those episodes, most people work, hang out with friends, travel, and do all the usual things.
Modern treatments have really changed how we approach it. Better medications and more specialists mean longer remission and better symptom control for a lot of people.
With good medical care and some self-management, you can stay independent and keep chasing your goals, even with IBD tagging along.
How To Manage It?
Managing IBD is about more than simply taking medication. It’s a whole-life approach focused on calming inflammation and putting out flares. There’s no cure, but you can absolutely take charge of the condition with the right strategies.
Medication Management
Taking your meds as prescribed is still the gold standard for keeping symptoms at bay. Finding the right combo can take some trial and error, so keep the conversation open with your doctor.
Dietary Modifications
Figuring out which foods set you off is a bit of a process. During flares, steer clear of anything that seems to make things worse, but don’t forget to keep your nutrition up.
A diet of easy-to-digest foods can make a real difference. Lots of people swear by keeping a food diary to spot patterns and triggers.
Lifestyle Changes
| Strategy | Benefit |
| Stress reduction | Helps prevent flares |
| Regular exercise | Boosts overall health |
| Adequate sleep | Keeps your immune system in check |
| Quitting smoking | Reduces inflammation |
Regular Monitoring
Keep your doctor in the loop about what’s working and what’s not. Being upfront about symptoms and flare-ups means your treatment can be tweaked as needed.
Nutritional Support
Fixing nutritional gaps is a big deal, since IBD can mess with absorption. Sometimes supplements are needed to keep your vitamin and mineral levels up.
And don’t forget about hydration,when you’re in a flare, you can lose fluids fast.
What Are The Treatments For Inflammatory Bowel Disease?
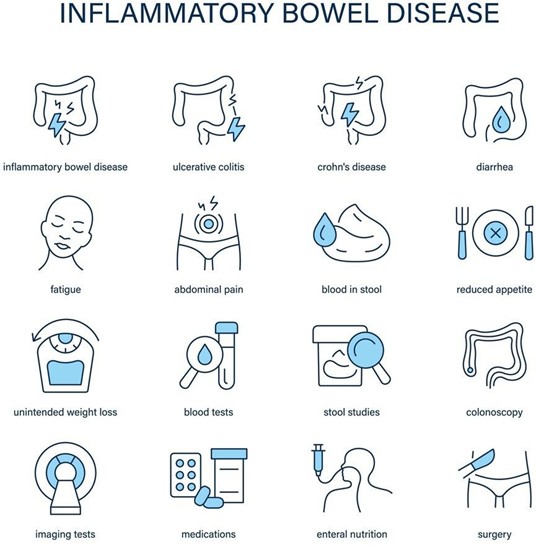
Treatments for IBD really depend on how severe your symptoms are and how your body reacts. There are a few main categories, each aiming to calm inflammation and keep symptoms in check.
Medication-Based Treatments
Aminosalicylates are usually the first stop for mild to moderate IBD. They’re anti-inflammatory and help keep things quiet in the gut.
Corticosteroids work fast during bad flares, but because of side effects, they’re not a long-term fix. Think of them more as a “get things under control” option.
Advanced Therapies
Biologics have truly revolutionized the treatment of IBD.. These meds target specific parts of the immune system and include things like TNF inhibitors and anti-integrin therapies.
JAK inhibitors are a newer oral option. Janus kinase inhibitors block inflammation signals inside cells, so you don’t need injections with these.
Ozanimod is another oral med that targets how immune cells move around, helping cut down inflammation in your gut. It’s one of the newer advances in biologic therapies.
| Treatment Type | Examples | Administration |
| Aminosalicylates | Mesalazine, Sulfasalazine | Oral/Rectal |
| Biologics | Infliximab, Adalimumab | Injection/Infusion |
| JAK Inhibitors | Tofacitinib | Oral |
Surgical Interventions
If meds just aren’t cutting it, surgery is sometimes needed. Colectomy (removing part or all of the colon) is most common in tough cases of ulcerative colitis.
Ultimately, treatment is very personal, what works for one person might not work for another. Most people end up using a mix of approaches to get the best results.
Conclusion
BD can’t be cured with anything modern medicine has to offer right now. It’s just something we have to live with—a chronic condition that demands lifelong attention, whether we like it or not.
But honestly, treatment has come a long way. We’re seeing therapies that do a solid job at keeping symptoms at bay and, for many, bring on long stretches of remission that would’ve seemed impossible a generation ago.
Here’s what really matters:
- There’s still no cure for Crohn’s disease or ulcerative colitis
- Remission can last months—or even years—if treatment’s on point
- Biologic drugs have changed the game for a lot of people
- Jumping in early with treatment can stop things from getting worse
- With the right care, quality of life can honestly be excellent
We keep hearing about new meds that look promising and are getting the green light from regulators. Plus, research into personalised medicine is picking up, so there’s hope for treatments that are more dialed-in to each person.
Current therapies aren’t perfect, sometimes they only partially work, and resistance can build up. Still, if you look back even a couple decades, the options now are almost hard to believe.
The focus isn’t just on tamping down symptoms anymore. Now, it’s about deep remission and actual healing of the gut lining, which really does seem to make a difference long-term.
So, no, we can’t cure IBD yet. But people can and do—live full, active lives. With a mix of advanced meds, lifestyle tweaks, and regular medical support, there’s plenty of reason to feel optimistic if you’re dealing with this.
FAQs
Can IBD be completely cured?
Not at the moment,there’s no known cure for IBD. Surgery can sometimes “cure” ulcerative colitis, but for most, it’s a lifelong deal.
What Diet Is Best For IBD?
There’s no magic diet that prevents or controls IBD for everyone. Still, tweaking what you eat can help manage symptoms, especially during flares or even in remission.
Is Inflammatory Bowel Disease Cancerous?
IBD itself isn’t cancerous. What we’re talking about are chronic inflammatory problems—Crohn’s and ulcerative colitis—that mess with the digestive tract.
Can Stress Cause IBD?
Bleeding can stop in certain instances after inflammation is alleviated. Recurring bleeding or excessive bleeding, however, requires medical care.
Stress doesn’t cause IBD outright, but it sure has a big impact on how the disease shows up and progresses. The real culprits are a mix of genetics, environment, and immune system quirks.
What Happens If Inflammatory Bowel Disease Is Left Untreated?
Letting IBD go untreated? That’s a recipe for some pretty serious health issues, honestly—things just tend to get worse the longer it’s ignored. Untreated inflammatory bowel disease can cause irreversible bowel damage and, frankly, it can really mess with your quality of life.

