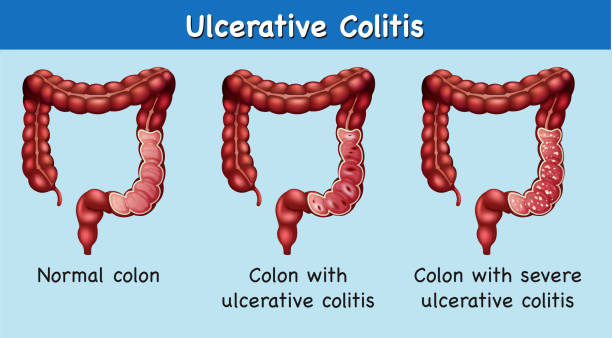
Ulcerative colitis is a long-term inflammation of the large intestine (colon) that causes irritation, tiny sores, and frequent digestive discomfort. It can come and go in cycles—periods of calm followed by flare-ups that bring symptoms like cramps or diarrhea.
Globally, studies suggest that around 0.3% to 0.5% of the population lives with ulcerative colitis, and more women in their childbearing years are now being diagnosed. In India, it’s estimated that about 10 out of every 100,000 people are affected, and awareness continues to rise in urban regions.
Dr. Ksheetij Kothari, a distinguished Gastroenterologist in Pune, explains:
“For most women, pregnancy doesn’t make ulcerative colitis worse. In fact, when the disease is under control before conception and monitored carefully throughout, the likelihood of a healthy pregnancy is very good. The real key is consistency—sticking to treatment and staying in touch with your medical team every step of the way.”
Let’s understand how ulcerative colitis interacts with pregnancy and what you can do to ensure both you and your baby remain healthy.
Maintaining a Healthy Pregnancy with Colitis
Many women with ulcerative colitis experience smooth, healthy pregnancies. The key factor lies in whether the disease is in remission when conception occurs.
Studies show that up to 80% of women with UC in remission at conception continue to stay stable throughout pregnancy. On the other hand, those who conceive during an active flare have a higher chance of ongoing symptoms or complications.
Here’s why remission makes such a difference:
Stable inflammation levels: Controlled inflammation means fewer immune disturbances that could affect implantation or fetal growth.
Better nutritional absorption: Stable gut function ensures you’re absorbing enough nutrients, vital for both you and your baby.
Reduced medication risks: With remission, you often need lower doses of medications, minimizing fetal exposure.
Dr. Kothari, a renowned ulcerative colitis specialist in Pune, emphasizes, “Planning your pregnancy during remission offers the best outcomes. It gives both mother and child a balanced environment to thrive. Even if flare-ups occur, timely management can keep complications minimal.”
But what happens if ulcerative colitis symptoms appear or worsen once you’re already pregnant? Let’s explore how this condition interacts with pregnancy itself.
The Impact of Ulcerative Colitis on Pregnancy
Pregnancy affects the immune system, hormones, and gut motility—all of which can influence UC. For some women, hormonal changes help keep inflammation down, while for others, the same shifts can trigger mild flare-ups.

Statistically, around 30% of women with UC may experience flare-ups during pregnancy, especially if their disease was active at conception. The most common symptoms include abdominal cramps, diarrhea, and occasional rectal bleeding.
Here’s what you might expect:
First Trimester: Some women notice mild flares as the body adjusts hormonally.
Second Trimester: Often the most stable phase, thanks to balanced hormone levels.
Third Trimester: A few may face renewed symptoms due to physical stress and digestive changes.
Dr. Kothari, an esteemed Gastroenterologist in Pune, notes, “Pregnancy naturally changes the immune response to protect the fetus. For UC patients, this can either bring relief or mild aggravation. What’s crucial is to stay in touch with your doctor, as timely medication adjustments prevent complications.”
Now that we’ve seen how UC interacts with pregnancy, it’s time to understand how you can take charge of your condition safely.
Managing Ulcerative Colitis during Pregnancy
Managing UC during pregnancy requires balance—protecting both the mother’s health and the baby’s safety. The good news is that most UC medications are safe during pregnancy when prescribed correctly. Stopping treatment abruptly can often cause more harm than continuing it.
Here’s how to maintain control:
Medication adherence: Drugs like mesalamine and certain corticosteroids are considered low-risk and help prevent flare-ups.
Nutritional care: Pregnancy increases nutritional demands. Focus on iron, folate, calcium, and omega-3s. A dietitian can tailor plans to prevent deficiencies.
Stress management: Pregnancy and UC both respond to stress. Gentle yoga, meditation, and regular sleep can make a difference.
Regular check-ups: Monitoring ensures medications remain safe and effective as pregnancy progresses.
Dr. Kothari, a leading Gastroenterologist in Pune, advises, “Avoid self-altering medication doses. Some mothers fear drug safety, but stopping therapy can cause flares, dehydration, and nutrient loss, which pose greater risks to the baby than most approved medications.”
Wondering what could go wrong if UC isn’t well managed during pregnancy? Let’s look at potential complications and how to minimize them.
Potential Risks and Complications
While many women deliver healthy babies, uncontrolled UC can raise risks. Awareness helps you act early.
Here are possible concerns:
Preterm Labor: Active UC can trigger early contractions, increasing chances of preterm birth.
Low Birth Weight: Poor nutrient absorption or inflammation can restrict fetal growth.
Increased C-section rates: Women with severe flares or rectal involvement may need surgical delivery for safety.
Medication side effects: Though rare, certain drugs may need adjustment to avoid affecting fetal development.
Globally, data shows that preterm birth risk is nearly twice as high in women with active UC compared to those in remission.
Dr. Kothari, a respected gastrointestinal specialist in Pune, states, “Early detection and prompt care reduce almost all major risks. If you’re attentive to symptoms and follow your medical plan, pregnancy outcomes are nearly identical to those without UC.”
Now that you know what to watch out for, how do you recognize when it’s time to reach out for medical help?
When to contact doctor
Don’t wait for symptoms to become overwhelming. Contact your doctor immediately if you notice:
Increased bowel movements or bleeding
Unexplained weight loss
Persistent fatigue or dehydration
Signs of infection or fever
Even mild flare-ups can escalate during pregnancy if untreated. Always err on the side of caution and communicate openly with your care team.
Conclusion
Pregnancy with UC may require extra attention, but it’s far from impossible. With modern treatments, continuous monitoring, and an informed approach, most women go on to deliver healthy babies and recover smoothly post-birth.
Dr. Kothari, a dedicated GI expert in Pune, concludes, “Pregnancy doesn’t have to be feared in women with ulcerative colitis. It’s about preparation, partnership, and persistence. When the disease is managed well, motherhood can be as joyful as ever.”
Let’s clear some common doubts so you can proceed with more clarity …
FAQs
Can ulcerative colitis cause a miscarriage?
While mild UC rarely leads to miscarriage, uncontrolled inflammation and dehydration can increase the risk. Staying in remission and managing flares early greatly reduces this possibility.
Can I pass ulcerative colitis to my baby?
UC isn’t directly inherited. However, genetic predisposition plays a role—your child may have a slightly higher risk, but lifestyle and environment matter far more.
Can ulcerative colitis affect your uterus?
UC primarily affects the colon, not the uterus. However, chronic inflammation and medications can influence hormonal balance or fertility temporarily.
Is breastfeeding safe with UC medications?
Yes, many UC drugs are compatible with breastfeeding. Always consult your doctor to confirm which medications are safe postpartum.
What can help prevent UC flare-ups during pregnancy?
Stay consistent with medications, maintain a nutrient-rich diet, manage stress, and attend regular prenatal and gastroenterology appointments. These steps can prevent most flare-ups effectively.
References:
https://my.clevelandclinic.org/health/diseases/10351-ulcerative-colitis
https://www.webmd.com/ibd-crohns-disease/ulcerative-colitis/uc-pregnancy-faqs
Disclaimer: The information shared in this content is for educational purposes only and not for promotional use.

